What is plantar fasciitis?
Have you ever woken up with foot pain at the worst possible time??
You have family in town, you are hosting and you need to get out of bed to start breakfast!
OUCH. NO! HOW? With your first step, your heel aches with a deep, unsettling pain. Last night you went to bed and your foot felt fine and now, out of nowhere, debilitating pain.
It improves slightly throughout the day, but you’re left with an annoying ache that stops you dead in your tracks of performing the activities you love. Exercise?
No way. Jogging? Walking to grab the mail or lifting up your child? Nope.
What’s responsible for your heel pain and misery?
Plantar fasciitis.
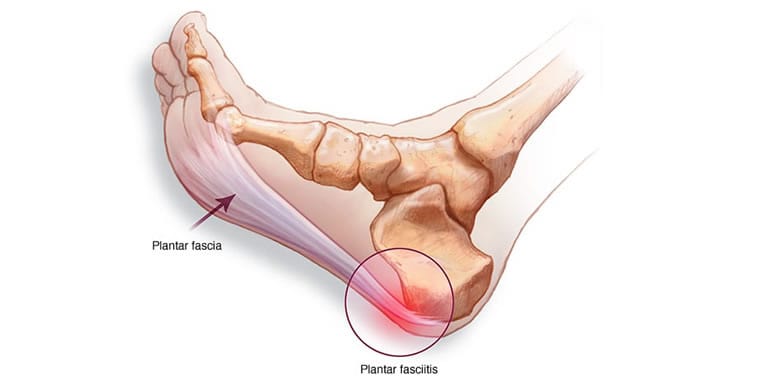
Plantar fasciitis is a painful condition caused by inflammation of the tissues in your foot and toes (“plantar” means “foot”, “fasciitis” means “inflamed fascia”). It is one of the most common causes of heel pain, accounting for 15% of all foot pain (1).
The bad news – it’s extremely painful and debilitating. The good news – we know the cause, symptoms, and how to fix it.
How do you know if you have plantar fasciitis?
The most common, “red flag” symptom of plantar fasciitis is heel pain that is worst in the morning or when walking after inactivity. That said, it presents differently in everyone.
Signs you may have plantar fasciitis include:
- Pain in the bottom of your foot
- “Stabbing” and “sharp” pain
- Pain that’s worse after inactivity (i.e. after sleep, work, or an 8 hour Harry Potter movie marathon with your kids)
- Pain that increases after exercise
- Heel pain without direct injury/trauma
If you’re experiencing one or more of these symptoms, you may have plantar fasciitis.
If your heel pain came out of nowhere, as if you were shot in the heel like a modern day Achilles, you’re not alone. While there often is not a single incident to blame, there are many common causes.
Most common causes of plantar fasciitis.
You’re at higher risk for plantar fasciitis if you:
- Are between 40-60 years old
- Have a job that requires you spend the majority of the day on your feet
- Have a body mass index >30 kg/m^2
- Recently increased activity levels, either with intentional exercise or work demands
- Reduced ankle dorsiflexion range of motion (the tighter your ankle, the higher your risk)
- Hip/glute weakness and instability
- Lack of triple extension through ankles, knees, and hips (if your glutes are weak, your calves will get overworked and tight)
Remember, you’re unique. It is possible that you don’t have any of these risk factors and still suffer from plantar fasciitis. If you’d like to know – once and for all – what’s causing your pain and how to fix it – Click here for more information about our approach to a whole host of foot and ankle issues.
You have plantar fasciitis. What do you do now? (Or should I say, how do you heal your heel?)
If you have plantar fasciitis, you’re probably thinking, in no particular order, “ouch!” and “how the heck do I fix this?”
First, you’d like to get out of pain. Next, you want to figure out how to prevent the pain from coming back in the future. Finally, you’d like to get back to your favorite activities without risking further injury.
Sound like a plan? Here’s how to fix your acute (short term) pain today.
How to immediately reduce your heel pain.
Remember, plantar fasciitis is inflammation of the fascia (connective tissue) in and around your foot. To reduce pain we need to reduce inflammation and increase blood flow to accelerate healing.
Inflammation is a vital component of your body’s natural healing response but in the acute phase (<48 hours) after an injury, it can cause more harm than good. If it’s within the first two days after injury, apply ice to the area to reduce pain and inflammation.
After the acute phase, you need to shift your focus to heat and activity – increasing blood flow, facilitating recovery, and increasing length through the tight tissues in your foot.
Here are 4 ways to reduce your plantar fasciitis pain:
- ce (within the first 24-48 hours) and then heat (after 48 hours) - Ice will help control inflammation and reduce pain. Heat will improve blood flow and reduce muscular tightness. Apply for up to 20 minutes 2-4x/day
- Self myofascial release with golf ball/lacrosse ball - Roll out the bottom of your foot by applying slow and sustained pressure along the bottom of your foot and into your heel. Perform for 1 minute each foot, 2-3x/day.
- Calf roll out - Put a lacrosse ball in between your hamstring and calf and roll out your calf muscles. Find a tight spot and hold the pressure for 60 seconds. Take deep breaths and, this is much easier said than done, do your best to relax while applying pressure. Repeat on both sides 2-3x/day.
- Calf stretch - Stretch your calf with your leg straight for 30 seconds, then move your foot up a few inches, bend your knee, and stretch your calf with your leg bent for 30 seconds. Stretching with a straight leg targets your Gastrocnemius and stretching with a bent leg targets your Soleus. Perform on both sides 2-3x/day.
How to prevent future injury.
This concept is difficult to wrap your head around but gets you closer to understanding the root cause of your pain.
Addressing your larger muscles closer to the midline of your body (shoulders, upper back, core, glutes), to fix pain in your smaller muscles and joints (feet/calves, forearms/biceps/triceps, knees/elbows is called a proximal to distal approach.” It is the best way to solve the root of your dysfunction and keep you out of pain.
Tennis/golfer’s elbow? Weakness and instability in your shoulder blades may be the cause.
Knee pain? Tightness and/or weakness in your hips and tightness in your ankles could be to blame.
With plantar fasciitis – and foot pain, in general – lack of strength, stability, and mobility in your hips is likely the cause.
After reducing your pain and improving the strength and mobility of your feet/ankles, look to your hips and glutes.
Here are 4 exercises that will improve your hip mobility (All Videos can be found on Instagram @DrJRuzicka_RPM):
- Hamstring roll out
- Glute roll out
- World’s greatest stretch
- Active pigeon
After increasing blood flow, loosening up your tissue and improving your range of motion, you’re ready to strengthen. Stronger glutes = more stable hips = happy feet and happy you!
Here are the top 4 movements we’ve found to strengthen your glutes without hurting your back or knees (hello strong glutes, goodbye Icy Hot and Advil). Find examples of these on Instagram for call our office for more information, these exercises are a great building block to increasing triple extension and taking pressure off the foot.
- Hip hinge squat
- Single leg toe tap
- Clam shells
- Side lying straight leg raise
If you have any questions or need to know which movements will be best for your body and goals, reach out to us with questions or comment on our social media page and we will answer them as soon as possible.
Will orthotics fix your heel pain?
I know exactly what you’re thinking – that all sounds fine and dandy, but can’t I just throw an orthotic in my shoe and call it a day?
Orthotics can reduce pain by correcting the alignment of the foot and redistributing pressure when you stand, walk or run. They have been shown to reduce pain (2) and are a low risk option to try if no other treatment is giving you relief.
Here’s the kicker – While the right orthotic may reduce your pain in the short term, they are not a long term fix. Wouldn’t you prefer this issue to go away entirely??
The long term solution
Orthotics, cortisone shots, anti-inflammatory and pain-relieving medication are “band aids” that will help your pain for a few days or weeks. They are useful tools in specific, short term situations. If you need to play in your championship game or enjoy a beach vacation without debilitating pain, take advantage of these options.
However, they will never fix the root cause of your pain. The best orthotic and strongest pain meds in the world can’t hold a candle to the long term relief and peace of mind that high quality physical therapy and direct knowledge on comprehensive solutions will give you.
The true long term fix. How to fix your pain and keep it gone.
You’re now equipped with the valuable tools you need to diagnose and treat your plantar fasciitis. With that said…
“The tool is only as effective as the skillfulness of the hands that wield it.”
- Joshua Ibiyinka
Here at RPM Physical Therapy and Performance, we have highly skilled physical therapists that will devise the most effective rehab plan for you. Through a combination of hands-on soft tissue work, dry needling, and targeted strength and mobility work, we will help you get back to the activities you love without pain.
Best of all, we give you the power. We’ll teach you how to fix your pain and prevent it from coming back.
The path to fixing your pain starts now. Call (713) 992-5916 or click the link below to schedule your free discovery visit with one of our physical therapists today.
Committed to your Health and Recovery,
Dr. John Solokas PT, DPT and Dr. Jonathan Ruzicka PT, DPT, FAAOMPT
Dr. Jonathan Ruzicka is a Manual Therapist whose experience as a private therapist for professional athletes drove him to further his education attaining unparalleled skills in tissue mobility work, performance based rehab, injury prevention, myofacial release and joint mobilization to optimize human performance.
- Physical Therapy for Oak Ridge North Residents Near The Woodlands - November 7, 2025
- Understanding Hip Pain: Causes, Treatment Options, and How to Protect Your Hips for the Long Term - September 30, 2025
- Improving Hip Mobility to Prepare for Colder Seasons - September 23, 2025


